Our Veterans have made tremendous sacrifices to defend our freedoms. Now it is our time to defend them.
Many people, even those who work in the operating room every day, take safe anesthesia care for granted. There has been growing pressure during this pandemic to remove physician supervision of nurse anesthetists with the latest threat coming from within Veterans Affairs (VA) healthcare. For our Veterans, our heroes and arguably some of the most medically complex patients, having a physician in charge of anesthesia care at hospitals where anesthesiologists and nurse anesthetists work together as a team makes the most sense.
Having a team with members who train differently and have different perspectives can only benefit the patient; anesthesiologists are physicians who draw on their medical training while nurse anesthetists bring valuable nursing experience. If you were a patient having surgery, wouldn’t you want an anesthesiologist directly involved in your care and leading the anesthesia team? If the answer is yes, please send your comments to Safe VA Care and let your elected officials know by contacting them.
Continue reading Beyond COVID-19: Stand Up for Veterans Having SurgeryProviding anesthesia is often compared to flying a passenger airplane, and the anesthesia care team model is like having both a pilot and a co-pilot.
Who thinks flying has become so safe that we no longer need the pilot? Seconds count in flight, and they count just as much in the operating room when a patient’s life is on the line.
In 2016, the VA rejected independent practice for nurse anesthetists after careful consideration, but this decision was recently overturned by a memo citing the COVID-19 pandemic. This memo abolishes the anesthesia care team model without giving Veterans a choice. Veterans having surgery may only get a nurse anesthetist without the option of having an anesthesiologist involved. If they were given the choice, however, I think our Veterans would choose an anesthesiologist or an anesthesia care team led by an anesthesiologist instead of a nurse anesthetist alone. We all should. In areas affected by surges of COVID-19, elective surgeries at the VA are stopped so there is no shortage of anesthesiologists.
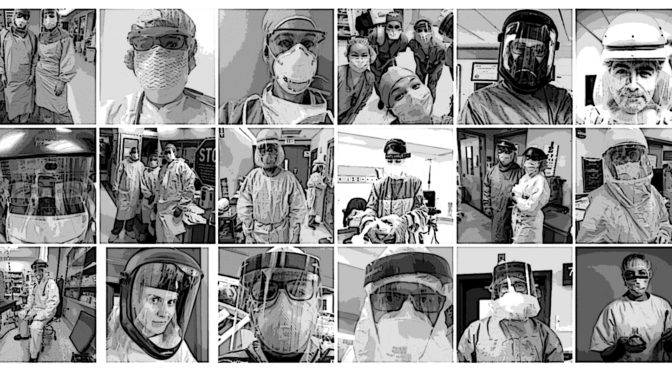
Anesthesiologists all over the world have been fighting COVID-19 and have shown what they can do with their specialized medical training in a crisis. Although commonly referred to as “going to sleep,” general anesthesia is more like a complex drug-induced coma that can carry serious risk. If or when a crisis happens during surgery, every patient should have access to an anesthesiologist.
Modern anesthesiologists are physicians first but also scientists, educators, and patient safety advocates. Anesthesiologists specialize in relieving anxiety, preventing and treating pain, preventing and managing complications related to surgery, critical care, and improving patient outcomes. The average anesthesiologist spends nearly a decade in postgraduate education after college including medical school and logs 16,000 hours of clinical training to learn to apply the best available evidence in clinical practice. Academic physicians and scientists focused on anesthesiology are responsible for the discovery of newer and safer anesthetics, pain therapies, and technologies that are advancing healthcare throughout the world.
Anesthesia administration by non-physicians such as nurse anesthetists and certified anesthesiologist assistants is supported by the American Society of Anesthesiologists within the physician-led anesthesia care team model. To uphold the highest quality physician-led anesthesia care for our nation’s Veterans, please speak up by supporting Safe VA Care and reaching out to legislators.
It only takes a minute to stand up for safety, but the consequences of not saying something may be serious and long-lasting.

 Many people, even those who work in the operating room every day, take safe anesthesia care for granted. There has been growing pressure recently to abandon the team model and remove physician anesthesiologists’ supervision of nurse anesthetists with the latest threat coming from within
Many people, even those who work in the operating room every day, take safe anesthesia care for granted. There has been growing pressure recently to abandon the team model and remove physician anesthesiologists’ supervision of nurse anesthetists with the latest threat coming from within 
