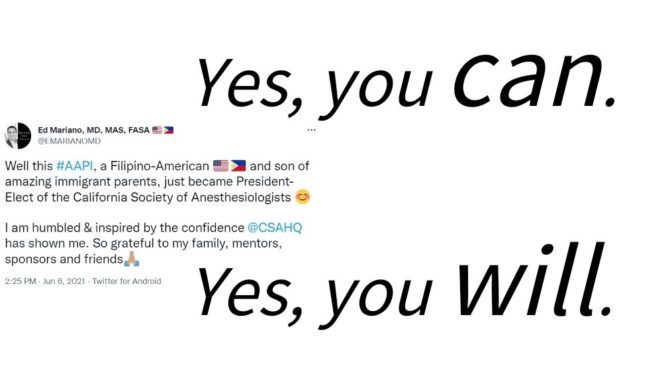
At the first in-person House of Delegates (HOD) session since 2019, I became President of the California Society of Anesthesiologists (CSA), the first Filipino-American to do so. This could have only happened because of the incredible mentors and sponsors that I have been fortunate enough to have in my life.
Over the course of the HOD weekend in June, we held a fundraising luncheon for the CSA Foundation, listened to project presentations from the first cohort of our CSA-UC Irvine Leadership in Healthcare Management Program launched by Drs. Phillip Richardson and Ron Pearl, were treated to a special guest lecture by Sasha Strauss on how to communicate as leaders and demonstrate value, and I provided an educational session on using social media for advocacy. We hosted Dr. Robert Wailes, President of the California Medical Association (CMA), for an update on the Medical Injury Compensation Reform Act (MICRA) since passage of AB 35 (MICRA Modernization). For more information, see Dr. Wailes’ summary.
During the HOD session, I outlined my leadership priorities for this year: expanding public-facing and internal member communications; continuing leadership development; planning the CSA’s 75th anniversary (diamond jubilee); and promoting wellbeing and professional fulfillment within the CSA membership. I discussed the challenges facing anesthesiology and the importance of recruiting and retaining members. I summarized the value proposition as “Community, Solidarity, and Advocacy,” which also happen to have the acronym “C-S-A.”


We followed HOD with our first Board of Directors (BOD) meeting of the governance year. We welcomed new Directors, appointed the CSA delegations to the American Society of Anesthesiologists (ASA) and CMA, and approved committee appointments for this governance year including an expanded Committee on Professional and Public Communication (CPPC). This new CPPC chaired by Dr. Emily Methangkool and staffed by Kate Peyser, and in partnership with Alison MacLeod and Lisa Yarbrough at KP Public Affairs, will be interfacing will all major committees, divisions, and task forces as well as the CSA Foundation to actively promote the great work by CSA members and advance the recognition, social standing, and influence of anesthesiologists.
Over the summer, I was Visiting Professor at the University of Michigan, hosted by Dr. Chad Brummett, and then had the privilege of participating in the American Medical Association (AMA) annual meeting as an ASA delegate to the AMA HOD. In this role, I was able to cast my vote for Dr. Jesse Ehrenfeld and witness him become the first anesthesiologist President-Elect of the AMA!


My family and I visited Greece for the first time as I participated as a guest speaker at the European Society of Regional Anaesthesia and Pain Therapy (ESRA) congress in Thessaloniki, and I also welcomed attendees to my first CSA educational event as President: the 2022 CSA Summer Anesthesia Conference. This meeting was chaired by Dr. Brendan Carvalho and featured a superstar all-women expert panel of dynamic speakers: Drs. Dalia Banks, Sapna Kudchadkar, Alana Flexman, BobbieJean Sweitzer, Romy Yun, and Elizabeth Ozery. All week, attendees and speakers engaged in conversations related to the practice of anesthesiology, caught up with old friends, and made new connections within the meeting room and around the resort. It was an amazing week of learning and family time and reinforced the value of CSA and its educational events in fostering community.


Before leaving Hawaii, I participated in a face-to-face meeting of the Hawaii Safer Care initiative, part of the Improving Surgical Care and Recovery collaborative supported by the Agency for Healthcare Quality and Research, and led by Dr. Della Lin, Senior Fellow in Patient Safety Leadership with the Estes Park Institute and is an inaugural National Patient Safety Foundation/Health Forums Patient Safety Leadership Fellow. Dr. Lin invited me to participate as a virtual coach during the pandemic last year and work with improvement teams focused on implementing multimodal pain management for surgical patients, so this was my first time meeting the group in person. For this meeting, teams from three statewide health systems within Hawaii reported out the results of their projects. The leadership and collaboration among the multidisciplinary teams to implement change despite the challenges of variable resource availability, staffing, and inter-island coordination could serve as a model to inspire our statewide efforts within CSA.
What do we have on deck for CSA?
At the time of this report, we are receiving applications for the next CSA-UC Irvine Leadership in Healthcare Management Program cohort. Anyone interested can sign up here. We have appointed the task forces to work on revamping the CSA website and planning activities for the 75th anniversary, including a family-friendly reception at the Annual Meeting in San Diego (April 27-30, 2023) that will be chaired by Dr. Christina Menor. Stay up to date with CSA events through our online calendar. Then in October, our CSA delegation heads to New Orleans for the ASA annual meeting, and CSA members will actively participate in educational programming, committee deliberations, and governance activities. CSA will host a member reception during the conference, and our delegates will stand proudly when CSA’s very own Dr. Michael Champeau takes over as President of the ASA at the conclusion of the Wednesday ASA HOD session!








 ternet, it is more important than ever for us to reach out to them.
ternet, it is more important than ever for us to reach out to them. Welcome to EdMariano.com!
Welcome to EdMariano.com!