I have written previously about what I love about being an anesthesiologist and why I still love being an anesthesiologist after all these years.
Recent articles have drawn attention to the pervasive problem of burnout among anesthesiologists, and the numbers are alarming. The overall prevalence within anesthesiology is approximately 60%, and this rate varies by subspecialty with pain physicians being at highest risk.
Our writing group has published two letters in the Journal of Clinical Anesthesia that offer additional perspectives and highlight important work on this subject: “A field on fire: Why has there been so much attention focused on burnout among anesthesiologists?” and “Fighting burnout in the COVID-19 era is a family matter.”
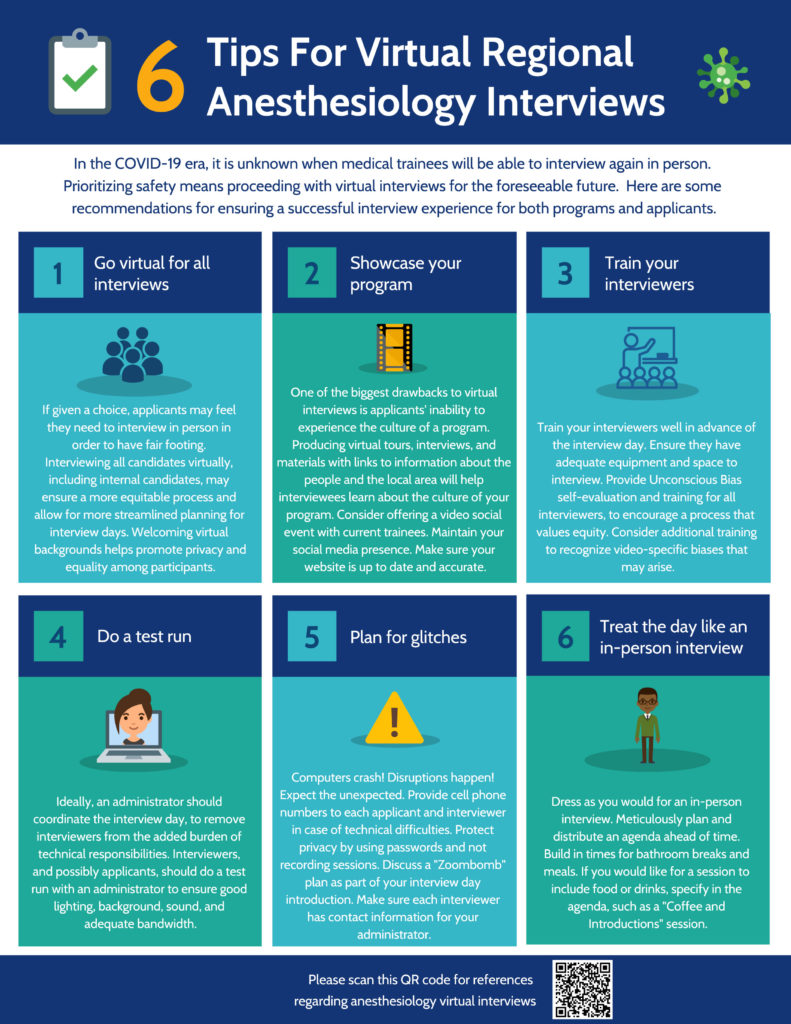
The previously-published studies by Hyman et al and Afonso et al report data collected prior to the onset of the COVID-19 pandemic. While anesthesiologists were hailed as frontline heroes worldwide for their roles in the emergency response, airway management, and critical care of COVID-19 patients, their lives and their careers were also completely disrupted.
At work, anesthesiologists had to deal with confronting a previously unknown and highly transmissible respiratory pandemic, long hours and uncertain schedules, new personal protective equipment (PPE) protocols and PPE shortages, quarantines, and frequently-changing guidelines. Shelter-in-place orders led to school and office closures which added the stressors of working from home and virtual schooling on top of pandemic parenting, and women anesthesiologists were disproportionately affected.
Moving forward, the ongoing assessment and mitigation of burnout among anesthesiologists will take dedicated effort and leadership. Our letter recommends periodic evaluation of work-related risk factors and check-ins with anesthesiologist team members. Further, recognition of the challenges to work-life integration imposed by the COVID-19 pandemic warrants implementation of reliable interventions that may prevent the same issues from happening again in the future.
In addition, it may be more appropriate to promote wellness at the family level, rather than simply the individual level, because anesthesiologists cannot reasonably focus on their important physician roles when there are concurrent and competing stressors at home.